感染利什曼原虫的雌性白蛉叮咬宿主时,将利什曼原虫前鞭毛体随白蛉唾液进入宿主皮下组织。[3]Killick-Kendrick R. The biology and control of phlebotomine sand flies. Clin Dermatol. 1999;17:279-289.http://www.ncbi.nlm.nih.gov/pubmed/10384867?tool=bestpractice.com一部分前鞭毛体可被多核白细胞吞噬消灭;一部分则进入巨噬细胞。[29]Rogers ME, Ilg T, Nikolaev AV, et al. Transmission of cutaneous leishmaniasis by sand flies is enhanced by regurgitation of fPPG. Nature. 2004;430:463-467.http://www.ncbi.nlm.nih.gov/pubmed/15269771?tool=bestpractice.com[30]Vannier-Santos MA, Martiny A, de Souza W. Cell biology of Leishmania spp.: invading and evading. Curr Pharm Des. 2002;8:297-318.http://www.ncbi.nlm.nih.gov/pubmed/11860368?tool=bestpractice.com [Figure caption and citation for the preceding image starts]: 静食白蛉图像由 CDC 提供;F. Collins [Citation ends].
[Figure caption and citation for the preceding image starts]: 静食白蛉图像由 CDC 提供;F. Collins [Citation ends].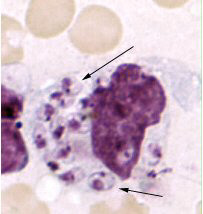 [Figure caption and citation for the preceding image starts]: 皮肤受损组织样本中的热带利什曼原虫无鞭毛体。整个巨噬细胞实际上充满了无鞭毛体,其中若干无鞭毛体拥有清晰可见的细胞核和动基体(箭头所示)图像由 CDC 提供;NCID;DPDx [Citation ends].试验研究表明,白蛉唾液可能将 Th1 型细胞介导的免疫反应转变为 Th2 型,从而导致血管舒张、红疹扩大、增加虫荷和、病灶面积和寄生虫滞留。[31]Kamhawi S. The biological and immunomodulatory properties of sand fly saliva and its role in the establishment of Leishmania infections. Microbes Infect. 2000;2:1765-1773.http://www.ncbi.nlm.nih.gov/pubmed/11137049?tool=bestpractice.com[32]Belkaid Y, Valenzuela JG, Kamhawi S, et al. Delayed-type hypersensitivity to Phlebotomus papatasi sand fly bite: an adaptive response induced by the fly? Proc Natl Acad Sci U S A. 2000;97:6704-6709.http://www.pnas.org/content/97/12/6704.fullhttp://www.ncbi.nlm.nih.gov/pubmed/10841567?tool=bestpractice.com自然环境内可用的一些有限数据表明,白蛉唾液的差异将决定婴儿利什曼原虫感染后的临床表现。[33]Warburg A, Saraiva E, Lanzaro GC, et al. Saliva of Lutzomyia longipalpis sibling species differs in its composition and capacity to enhance leishmaniasis. Philos Trans R Soc Lond B. 1994;345:223-230.http://www.ncbi.nlm.nih.gov/pubmed/7972360?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: 皮肤受损组织样本中的热带利什曼原虫无鞭毛体。整个巨噬细胞实际上充满了无鞭毛体,其中若干无鞭毛体拥有清晰可见的细胞核和动基体(箭头所示)图像由 CDC 提供;NCID;DPDx [Citation ends].试验研究表明,白蛉唾液可能将 Th1 型细胞介导的免疫反应转变为 Th2 型,从而导致血管舒张、红疹扩大、增加虫荷和、病灶面积和寄生虫滞留。[31]Kamhawi S. The biological and immunomodulatory properties of sand fly saliva and its role in the establishment of Leishmania infections. Microbes Infect. 2000;2:1765-1773.http://www.ncbi.nlm.nih.gov/pubmed/11137049?tool=bestpractice.com[32]Belkaid Y, Valenzuela JG, Kamhawi S, et al. Delayed-type hypersensitivity to Phlebotomus papatasi sand fly bite: an adaptive response induced by the fly? Proc Natl Acad Sci U S A. 2000;97:6704-6709.http://www.pnas.org/content/97/12/6704.fullhttp://www.ncbi.nlm.nih.gov/pubmed/10841567?tool=bestpractice.com自然环境内可用的一些有限数据表明,白蛉唾液的差异将决定婴儿利什曼原虫感染后的临床表现。[33]Warburg A, Saraiva E, Lanzaro GC, et al. Saliva of Lutzomyia longipalpis sibling species differs in its composition and capacity to enhance leishmaniasis. Philos Trans R Soc Lond B. 1994;345:223-230.http://www.ncbi.nlm.nih.gov/pubmed/7972360?tool=bestpractice.com
在巨噬细胞的吞噬溶酶体内,前鞭毛体会转变为无鞭毛体。[34]Basu MK, Ray M. Macrophage and Leishmania: an unacceptable coexistence. Crit Rev Microbiol. 2005;31:145-154.http://www.ncbi.nlm.nih.gov/pubmed/16170905?tool=bestpractice.com [Figure caption and citation for the preceding image starts]: 利什曼原虫的生活史,利什曼病的病原体图像由 CDC 提供;A.J. da Silva, PhD;M. Moser [Citation ends].无鞭毛体进行分裂繁殖,导致巨噬细胞破裂。游离的无鞭毛体可在附近又进入其他巨噬细胞(如局限性皮肤利什曼病),或播散到远端组织内的巨噬细胞中(如内脏或黏膜利什曼病)。目前尚不清楚一些利什曼原虫虫种会局限在叮咬处,而某些虫种会播散到其他部位。[1]Reithinger R, Dujardin JC, Louzir H, et al. Cutaneous leishmaniasis. Lancet Infect Dis. 2007;7:581-596.http://www.ncbi.nlm.nih.gov/pubmed/17714672?tool=bestpractice.com[2]Chappuis F, Sundar S, Hailu A, et al. Visceral leishmaniasis: what are the needs for diagnosis, treatment and control? Nat Rev Microbiol. 2007;5:873-882, S7-S16.http://www.ncbi.nlm.nih.gov/pubmed/17938629?tool=bestpractice.com进入皮下组织的利什曼原虫可藉淋巴和血管系统播散到其他部位,引起其他部位的单核细胞和巨噬细胞感染。继而引起骨髓浸润、肝脾肿大,有时还会引起淋巴结肿大。
[Figure caption and citation for the preceding image starts]: 利什曼原虫的生活史,利什曼病的病原体图像由 CDC 提供;A.J. da Silva, PhD;M. Moser [Citation ends].无鞭毛体进行分裂繁殖,导致巨噬细胞破裂。游离的无鞭毛体可在附近又进入其他巨噬细胞(如局限性皮肤利什曼病),或播散到远端组织内的巨噬细胞中(如内脏或黏膜利什曼病)。目前尚不清楚一些利什曼原虫虫种会局限在叮咬处,而某些虫种会播散到其他部位。[1]Reithinger R, Dujardin JC, Louzir H, et al. Cutaneous leishmaniasis. Lancet Infect Dis. 2007;7:581-596.http://www.ncbi.nlm.nih.gov/pubmed/17714672?tool=bestpractice.com[2]Chappuis F, Sundar S, Hailu A, et al. Visceral leishmaniasis: what are the needs for diagnosis, treatment and control? Nat Rev Microbiol. 2007;5:873-882, S7-S16.http://www.ncbi.nlm.nih.gov/pubmed/17938629?tool=bestpractice.com进入皮下组织的利什曼原虫可藉淋巴和血管系统播散到其他部位,引起其他部位的单核细胞和巨噬细胞感染。继而引起骨髓浸润、肝脾肿大,有时还会引起淋巴结肿大。
在晚期内脏利什曼病中,骨髓和脾脏浸润会造成血细胞生成量减少,消耗量增加(脾功能亢进)。从而引起贫血、血小板减少症和/或白细胞减少症。当网状内皮系统被侵袭后,单核细胞系变得越来越易受其他传染源感染,表现为高频率的叠加细菌感染(如肺炎、腹泻或肺结核)。
多数人在感染利什曼原虫后呈无症状的状态。[1]Reithinger R, Dujardin JC, Louzir H, et al. Cutaneous leishmaniasis. Lancet Infect Dis. 2007;7:581-596.http://www.ncbi.nlm.nih.gov/pubmed/17714672?tool=bestpractice.com[2]Chappuis F, Sundar S, Hailu A, et al. Visceral leishmaniasis: what are the needs for diagnosis, treatment and control? Nat Rev Microbiol. 2007;5:873-882, S7-S16.http://www.ncbi.nlm.nih.gov/pubmed/17938629?tool=bestpractice.com无症状感染和感染后出现症状的比率取决于感染的利什曼原虫的种株、宿主和白蛉的因素以及其他非典型因素。例如,以婴儿利什曼原虫为病原体的内脏利什曼病流行区人群中无症状感染的比率高于以杜氏利什曼原虫为病原体的内脏利什曼病流行区,由此可见,后一种利什曼原虫的毒力更高。有研究表明,拉丁美洲的人群中婴儿利什曼原虫无症状感染和出现症状的比率与欧洲不同,可能由于对感染和疾病产生影响的其他因素(如营养不良)所致。[2]Chappuis F, Sundar S, Hailu A, et al. Visceral leishmaniasis: what are the needs for diagnosis, treatment and control? Nat Rev Microbiol. 2007;5:873-882, S7-S16.http://www.ncbi.nlm.nih.gov/pubmed/17938629?tool=bestpractice.com细胞介导免疫缺陷的人,如 HIV 感染的人或重度营养不良的人患该疾病的风险会更高,并且有时会在感染后的数年或数十年后发病。[17]Alvar J, Aparicio P, Aseffa A, et al. The relationship between leishmaniasis and AIDS: the second 10 years. Clin Microbiol Rev. 2008;21:334-359.http://cmr.asm.org/content/21/2/334.fullhttp://www.ncbi.nlm.nih.gov/pubmed/18400800?tool=bestpractice.com[35]Cerf BJ, Jones TC, Badaro R, et al. Malnutrition as a risk factor for severe visceral leishmaniasis. J Infect Dis. 1987;156:1030-1033.http://www.ncbi.nlm.nih.gov/pubmed/3680989?tool=bestpractice.com[36]Murray HW. Kala-azar as an AIDS-related opportunistic infection. AIDS Patient Care STDS. 1999;13:459-465.http://www.ncbi.nlm.nih.gov/pubmed/10800524?tool=bestpractice.com其他有关由宿主决定的因素(如遗传因素)可能在适应性免疫反应中起到重要作用。[27]Handman E, Elso C, Foote S. Genes and susceptibility to leishmaniasis. Adv Parasitol. 2005;59:1-75.http://www.ncbi.nlm.nih.gov/pubmed/16182864?tool=bestpractice.com
 [Figure caption and citation for the preceding image starts]: 静食白蛉图像由 CDC 提供;F. Collins [Citation ends].传播取决于该病的宿主是患者(人源型)还是感染原虫的哺乳动物(动物源型)。若干白蛉属的蛉种和哺乳动物物种分别为利什曼病的媒介和储存宿主。[1][2]其他传播方式(如先天性、输血、器官移植、实验室感染)虽然存在,但很罕见。[4][5]
[Figure caption and citation for the preceding image starts]: 静食白蛉图像由 CDC 提供;F. Collins [Citation ends].传播取决于该病的宿主是患者(人源型)还是感染原虫的哺乳动物(动物源型)。若干白蛉属的蛉种和哺乳动物物种分别为利什曼病的媒介和储存宿主。[1][2]其他传播方式(如先天性、输血、器官移植、实验室感染)虽然存在,但很罕见。[4][5] [Figure caption and citation for the preceding image starts]: 静食白蛉图像由 CDC 提供;F. Collins [Citation ends].
[Figure caption and citation for the preceding image starts]: 静食白蛉图像由 CDC 提供;F. Collins [Citation ends].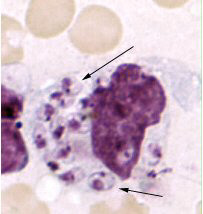 [Figure caption and citation for the preceding image starts]: 皮肤受损组织样本中的热带利什曼原虫无鞭毛体。整个巨噬细胞实际上充满了无鞭毛体,其中若干无鞭毛体拥有清晰可见的细胞核和动基体(箭头所示)图像由 CDC 提供;NCID;DPDx [Citation ends].试验研究表明,白蛉唾液可能将 Th1 型细胞介导的免疫反应转变为 Th2 型,从而导致血管舒张、红疹扩大、增加虫荷和、病灶面积和寄生虫滞留。[31][32]自然环境内可用的一些有限数据表明,白蛉唾液的差异将决定婴儿利什曼原虫感染后的临床表现。[33]
[Figure caption and citation for the preceding image starts]: 皮肤受损组织样本中的热带利什曼原虫无鞭毛体。整个巨噬细胞实际上充满了无鞭毛体,其中若干无鞭毛体拥有清晰可见的细胞核和动基体(箭头所示)图像由 CDC 提供;NCID;DPDx [Citation ends].试验研究表明,白蛉唾液可能将 Th1 型细胞介导的免疫反应转变为 Th2 型,从而导致血管舒张、红疹扩大、增加虫荷和、病灶面积和寄生虫滞留。[31][32]自然环境内可用的一些有限数据表明,白蛉唾液的差异将决定婴儿利什曼原虫感染后的临床表现。[33] [Figure caption and citation for the preceding image starts]: 利什曼原虫的生活史,利什曼病的病原体图像由 CDC 提供;A.J. da Silva, PhD;M. Moser [Citation ends].无鞭毛体进行分裂繁殖,导致巨噬细胞破裂。游离的无鞭毛体可在附近又进入其他巨噬细胞(如局限性皮肤利什曼病),或播散到远端组织内的巨噬细胞中(如内脏或黏膜利什曼病)。目前尚不清楚一些利什曼原虫虫种会局限在叮咬处,而某些虫种会播散到其他部位。[1][2]进入皮下组织的利什曼原虫可藉淋巴和血管系统播散到其他部位,引起其他部位的单核细胞和巨噬细胞感染。继而引起骨髓浸润、肝脾肿大,有时还会引起淋巴结肿大。
[Figure caption and citation for the preceding image starts]: 利什曼原虫的生活史,利什曼病的病原体图像由 CDC 提供;A.J. da Silva, PhD;M. Moser [Citation ends].无鞭毛体进行分裂繁殖,导致巨噬细胞破裂。游离的无鞭毛体可在附近又进入其他巨噬细胞(如局限性皮肤利什曼病),或播散到远端组织内的巨噬细胞中(如内脏或黏膜利什曼病)。目前尚不清楚一些利什曼原虫虫种会局限在叮咬处,而某些虫种会播散到其他部位。[1][2]进入皮下组织的利什曼原虫可藉淋巴和血管系统播散到其他部位,引起其他部位的单核细胞和巨噬细胞感染。继而引起骨髓浸润、肝脾肿大,有时还会引起淋巴结肿大。