初发的临床表现可从无症状至终末期肝病并发症表现。越来越多的患者是在体检时发现无症状的转氨酶升高。[2]Kaplan GG, Laupland KB, Butzner D, et al. The burden of large and small duct primary sclerosing cholangitis in adults and children: a population-based analysis. Am J Gastroenterol. 2007;102:1042-1049.http://www.ncbi.nlm.nih.gov/pubmed/17313496?tool=bestpractice.com[5]Bambha K, Kim WR, Talwalkar J, et al. Incidence, clinical spectrum, and outcomes of primary sclerosing cholangitis in a United States community. Gastroenterology. 2003;125:1364-1369.http://www.ncbi.nlm.nih.gov/pubmed/14598252?tool=bestpractice.com诊断主要依靠临床表现、胆汁瘀积性肝病检查和典型的胆管造影。然而,由于症状不明显以及隐匿起病,该病很难早期诊断。
诊断PSC需要排除继发性硬化性胆管炎(指其他原因导致的胆管异常和类似的临床和胆道造影综合征[如手术创伤、胆管结石、复发性胰腺炎、动脉内化疗损伤或肿瘤等])。[21]Abdalian R, Heathcote EJ. Sclerosing cholangitis: a focus on secondary causes. Hepatology. 2006;44:1063-1074.http://www.ncbi.nlm.nih.gov/pubmed/17058222?tool=bestpractice.com
突发的或明显恶化的症状或生化检查通常表明已有明显胆管狭窄或胆管癌。
晚期肝病或肝硬化的患者应及时就诊于肝移植中心进行评估和管理。
病史
半数患者无临床症状。[4]Kingham JG, Kochar N, Gravenor MB. Incidence, clinical patterns and outcomes of primary sclerosing cholangitis in South Wales, United Kingdom. Gastroenterology 2004;126:1929-1930.http://www.ncbi.nlm.nih.gov/pubmed/15188211?tool=bestpractice.com常见症状有乏力、上腹痛和皮肤瘙痒。乏力并非特异性表现,但通常患者诊断时多有乏力表现。[2]Kaplan GG, Laupland KB, Butzner D, et al. The burden of large and small duct primary sclerosing cholangitis in adults and children: a population-based analysis. Am J Gastroenterol. 2007;102:1042-1049.http://www.ncbi.nlm.nih.gov/pubmed/17313496?tool=bestpractice.com[10]Bergquist A, Said K, Broome U. Changes over a 20-year period in the clinical presentation of primary sclerosing cholangitis in Sweden. Scand J Gastroenterol. 2007;42:88-93.http://www.ncbi.nlm.nih.gov/pubmed/17190768?tool=bestpractice.com腹痛通常为非特异性表现,位于右上腹或上腹部。[2]Kaplan GG, Laupland KB, Butzner D, et al. The burden of large and small duct primary sclerosing cholangitis in adults and children: a population-based analysis. Am J Gastroenterol. 2007;102:1042-1049.http://www.ncbi.nlm.nih.gov/pubmed/17313496?tool=bestpractice.com[10]Bergquist A, Said K, Broome U. Changes over a 20-year period in the clinical presentation of primary sclerosing cholangitis in Sweden. Scand J Gastroenterol. 2007;42:88-93.http://www.ncbi.nlm.nih.gov/pubmed/17190768?tool=bestpractice.com[6]Tischendorf JJ, Hecker H, Kruger M, et al. Characterization, outcome, and prognosis in 273 patients with primary sclerosing cholangitis: a single center study. Am J Gastroenterol. 2007;102:107-114.http://www.ncbi.nlm.nih.gov/pubmed/17037993?tool=bestpractice.com皮肤瘙痒常为间歇性,然而可以加重甚至影响睡眠和日常活动。肝病患者可有皮肤黄染、大便色白,恶臭且排便困难,呕血、意识不清和腹围增加。
75%患者既往有炎症性肠病(典型表现为溃疡性结肠炎,但也可为克罗恩病)病史。[4]Kingham JG, Kochar N, Gravenor MB. Incidence, clinical patterns and outcomes of primary sclerosing cholangitis in South Wales, United Kingdom. Gastroenterology 2004;126:1929-1930.http://www.ncbi.nlm.nih.gov/pubmed/15188211?tool=bestpractice.com[5]Bambha K, Kim WR, Talwalkar J, et al. Incidence, clinical spectrum, and outcomes of primary sclerosing cholangitis in a United States community. Gastroenterology. 2003;125:1364-1369.http://www.ncbi.nlm.nih.gov/pubmed/14598252?tool=bestpractice.com[10]Bergquist A, Said K, Broome U. Changes over a 20-year period in the clinical presentation of primary sclerosing cholangitis in Sweden. Scand J Gastroenterol. 2007;42:88-93.http://www.ncbi.nlm.nih.gov/pubmed/17190768?tool=bestpractice.com[6]Tischendorf JJ, Hecker H, Kruger M, et al. Characterization, outcome, and prognosis in 273 patients with primary sclerosing cholangitis: a single center study. Am J Gastroenterol. 2007;102:107-114.http://www.ncbi.nlm.nih.gov/pubmed/17037993?tool=bestpractice.com研究表明肠镜活检示90%患者患有肠炎,在PSC诊断前后均可发病。[22]Tung BY, Brentnall T, Kowdley K, et al. Diagnosis and prevalence of ulcerative colitis in patients with sclerosing cholangitis (abstract). Hepatology. 1996;24:169A.炎症性肠病可在 PSC 之前或之后发病,[10]Bergquist A, Said K, Broome U. Changes over a 20-year period in the clinical presentation of primary sclerosing cholangitis in Sweden. Scand J Gastroenterol. 2007;42:88-93.http://www.ncbi.nlm.nih.gov/pubmed/17190768?tool=bestpractice.com并且频繁表现为除直肠以外的全结肠炎和倒灌性回肠炎。[20]Loftus EV Jr, Harewood GC, Loftus CG, et al. PSC-IBD: a unique form of inflammatory bowel disease associated with primary sclerosing cholangitis. Gut. 2005;54:91-96.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1774346/http://www.ncbi.nlm.nih.gov/pubmed/15591511?tool=bestpractice.com
查体
体检可有抓痕(有瘙痒的患者)、体重减轻(脂肪吸收不良、活动性炎症性肠病和/或终末期肝病)、黄疸、脾大、腹水、肝性脑病、食道静脉曲张出血和/或发热(间断细菌性胆管炎)。
实验室检查
PSC不能仅靠实验室检查诊断,但其具有指导意义(尤其是血清碱性磷酸酶的升高)。
肝功能检查
具有上述症状和即使无症状但有炎症性肠病病史的患者均需要进行检查。
常表现为胆汁淤积。
血清碱性磷酸酶来源于肝脏和骨骼。多数PSC患者血清碱性磷酸酶升高,8.5%患者可为正常,[23]Broome U, Olsson R, Loof L, et al. Natural history and prognostic factors in 305 Swedish patients with primary sclerosing cholangitis. Gut. 1996;38:610-615.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1383124/http://www.ncbi.nlm.nih.gov/pubmed/8707097?tool=bestpractice.com儿童中碱性磷酸酶正常的比例更高。[24]Wilschanski M, Chait P, Wade JA, et al. Primary sclerosing cholangitis in 32 children: clinical, laboratory, and radiographic features, with survival analysis. Hepatology. 1995;22:1415-1422.http://www.ncbi.nlm.nih.gov/pubmed/7590657?tool=bestpractice.com是否为肝源性的碱性磷酸酶升高可通过血清γ-GT的水平来判断,同时伴有γ-GT升高考虑肝病,而γ-GT不升高考虑骨性疾病。
多数患者有轻中度转氨酶升高(多为正常上限的2-3倍)。
胆红素在疾病早期波动,随着疾病进展逐渐加重。
大多数患者诊断明确时肝合成功能尚正常,因此白蛋白和凝血酶原时间可正常(可能由于合并有活动性炎症性肠病而致白蛋白下降)。
自身抗体
PSC无特异性或诊断性的自身抗体。然而实验室检查时很多自身免疫抗体是阳性的(如ANCA,ANA,抗平滑肌抗体和类风湿因子)。
在PSC患者中这些自身抗体的临床意义还不清楚。
自身免疫性肝炎和PSC患者血清中自身免疫抗体(ANA和抗平滑肌抗体)通常阳性,分别为8%至77%和0%至83%。[12]Hov JR, Boberg KM, Karlsen TH. Autoantibodies in primary sclerosing cholangitis. World J Gastroenterol. 2008;14:3781-3791.http://www.ncbi.nlm.nih.gov/pubmed/18609700?tool=bestpractice.com
重要的是这些自身免疫抗体缺乏特异性,对于那些临床表现与PSC相符的患者,即使这些抗体的阳性也不能除外诊断PSC或提示其他诊断。
PSC患者抗线粒体抗体是阴性的(原发性胆汁性肝硬化患者一般是阳性的)。
血清自身免疫抗体并不需要常规检查,但如果考虑原发性胆汁性肝硬化应检查抗线粒体抗体,而考虑PSC重叠免疫性肝炎的患者应检查ANA和抗平滑肌抗体。
其他实验室检查
免疫球蛋白
有病史和异常肝功能患者中免疫球蛋白阳性可能有自身免疫性肝炎或原发性胆汁性肝硬化。
IgG和IgM并不是PSC的基本评估指标,但二者之一升高且临床高度疑诊则不能排除PSC。
IgG升高常见于自身免疫性肝炎,IgM升高常见于原发性胆汁性肝硬化。[7]Boberg KM, Aadland E, Jahnsen J, et al. Incidence and prevalence of primary biliary cirrhosis, primary sclerosing cholangitis, and autoimmune hepatitis in a Norwegian population. Scand J Gastroenterol. 1998;33:99-103.http://www.ncbi.nlm.nih.gov/pubmed/9489916?tool=bestpractice.com
IgG4可在多器官性淋巴浆细胞性硬化病中升高,如硬化性胆管炎。IgG4相关性胆管炎常伴发自身免疫性胰腺炎,且对糖皮质激素治疗反应敏感。12%的PSC患者血清IgG4水平升高。建议将IgG4相关的PSC单独列为一型。建议所有怀疑PSC患者检查IgG4。[25]Chapman R, Fevery J, Kalloo A, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51:660-678.http://onlinelibrary.wiley.com/doi/10.1002/hep.23294/fullhttp://www.ncbi.nlm.nih.gov/pubmed/20101749?tool=bestpractice.com[26]Ghazale A, Chari ST, Zhang L, et al. Immunoglobulin G4-associated cholangitis: clinical profile and response to therapy. Gastroenterology. 2008;134:706-715.http://www.ncbi.nlm.nih.gov/pubmed/18222442?tool=bestpractice.com[27]Björnsson E, Chari S, Silveira M, et al. Primary sclerosing cholangitis associated with elevated immunoglobulin G4: clinical characteristics and response to therapy. Am J Ther. 2011;18:198-205.http://www.ncbi.nlm.nih.gov/pubmed/20228674?tool=bestpractice.com[28]Webster GJ, Pereira SP, Chapman RW. Autoimmune pancreatitis/IgG4-associated cholangitis and primary sclerosing cholangitis: overlapping or separate diseases? J Hepatol. 2009;51:398-402.http://www.ncbi.nlm.nih.gov/pubmed/19505739?tool=bestpractice.com[29]Ohara H, Okazaki K, Tsubouchi H, et al. Clinical diagnostic criteria of IgG4-related sclerosing cholangitis 2012. J Hepatobiliary Pancreat Sci. 2012;19:536-542.http://www.ncbi.nlm.nih.gov/pubmed/22717980?tool=bestpractice.com
铜
血浆铜蓝蛋白
影像学检查
胆道系统的影像学检查对于诊断PSC是必要的。
腹部超声
CT
CT成像可显示胆管增厚、局灶或囊性的肝内胆管扩张,或淋巴结肿大。亦可发现表现为肿块占位的胆管癌。[30]Walker SL, McCormick PA. Diagnosing cholangiocarcinoma in primary sclerosing cholangitis: an "evidence based radiology" review. Abdom Imaging. 2008;33:14-17.http://www.ncbi.nlm.nih.gov/pubmed/17874262?tool=bestpractice.com[31]Campbell WL, Peterson MS, Federle MP, et al. Using CT and cholangiography to diagnose biliary tract carcinoma complicating primary sclerosing cholangitis. AJR Am J Roentgenol. 2001;177:1095-1100.http://www.ajronline.org/content/177/5/1095.fullhttp://www.ncbi.nlm.nih.gov/pubmed/11641179?tool=bestpractice.com[32]Ament AE, Haaga JR, Wiedenmann SD, et al. Primary sclerosing cholangitis: CT findings. J Comput Assist Tomogr. 1983;7:795-800.http://www.ncbi.nlm.nih.gov/pubmed/6886129?tool=bestpractice.com
对那些反复出现临床症状和实验室检查提示有可能为恶性病变的患者来说CT检查是有意义的。
胆管造影
磁共振胰胆管成像(MRCP)或经内镜逆行性胰胆管造影术(ERCP)检查对于明确胆道病变是较好的影像检查方法。
PSC患者胆管造影显示为小胆管紊乱,肝内胆管分支减少、狭窄,肝内外胆管多灶性的狭窄,呈串珠样改变。当然,肝内胆管分支减少也可见于各种原因所致的肝硬化。[33]Terada T, Nakanuma Y. Intrahepatic cholangiographic appearance simulating primary sclerosing cholangitis in several hepatobiliary diseases: a postmortem cholangiographic and histopathological study in 154 livers at autopsy. Hepatology. 1995;22:75-81.http://www.ncbi.nlm.nih.gov/pubmed/7601436?tool=bestpractice.com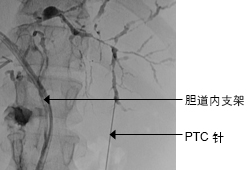 [Figure caption and citation for the preceding image starts]: 某患者的ERCP典型表现:肝内外胆管的多灶性狭窄Dr Kris Kowdley 收藏的资料 [Citation ends].
[Figure caption and citation for the preceding image starts]: 某患者的ERCP典型表现:肝内外胆管的多灶性狭窄Dr Kris Kowdley 收藏的资料 [Citation ends].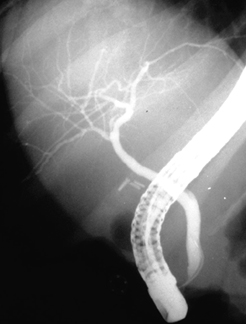 [Figure caption and citation for the preceding image starts]: 正常ECCPDr Michael Saunders 收藏的资料 [Citation ends].
[Figure caption and citation for the preceding image starts]: 正常ECCPDr Michael Saunders 收藏的资料 [Citation ends]. [Figure caption and citation for the preceding image starts]: 正常胆管造影-胰腺造影图Dr Michael Saunders 收藏的资料 [Citation ends].
[Figure caption and citation for the preceding image starts]: 正常胆管造影-胰腺造影图Dr Michael Saunders 收藏的资料 [Citation ends].
ERCP和MRCP都有助于疾病诊断并能评估疾病程度。
MRCP为无创性检查手段,是与ERCP相似的高敏感性和特异性的检查。[34]Dave M, Elmunzer BJ, Dwamena BA, et al. Primary sclerosing cholangitis: meta-analysis of diagnostic performance of MR cholangiopancreatography. Radiology. 2010;256:387-396.http://radiology.rsna.org/content/256/2/387.longhttp://www.ncbi.nlm.nih.gov/pubmed/20656832?tool=bestpractice.com对于无症状、少或无胆汁淤积且无需治疗干预的患者可行此检查,对于MRCP无法确诊或需要治疗干预(如高度怀疑胆总管狭窄或胆管癌)的患者则需选择ERCP检查。[35]European Association for the Study of the Liver. EASL clinical practice guidelines: management of cholestatic liver diseases. J Hepatol. 2009;51:237-267.http://www.easl.eu/research/our-contributions/clinical-practice-guidelines/detail/management-of-cholestatic-liver-diseaseshttp://www.ncbi.nlm.nih.gov/pubmed/19501929?tool=bestpractice.com[34]Dave M, Elmunzer BJ, Dwamena BA, et al. Primary sclerosing cholangitis: meta-analysis of diagnostic performance of MR cholangiopancreatography. Radiology. 2010;256:387-396.http://radiology.rsna.org/content/256/2/387.longhttp://www.ncbi.nlm.nih.gov/pubmed/20656832?tool=bestpractice.com[25]Chapman R, Fevery J, Kalloo A, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51:660-678.http://onlinelibrary.wiley.com/doi/10.1002/hep.23294/fullhttp://www.ncbi.nlm.nih.gov/pubmed/20101749?tool=bestpractice.com
ERCP为PSC的确诊手段。然而,这种侵入性检查手段导致多种并发症的风险,包括胰腺炎、出血、胆管炎和胆管穿孔。[25]Chapman R, Fevery J, Kalloo A, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51:660-678.http://onlinelibrary.wiley.com/doi/10.1002/hep.23294/fullhttp://www.ncbi.nlm.nih.gov/pubmed/20101749?tool=bestpractice.com[36]de Rougemont O, Dutkowski P, Clavien PA. Clinical update on inflammatory disorders of the GI tract: liver transplantation. In: Mayerle J, Tilg H, eds. Clinical update on inflammatory disorders of the gastrointestinal tract. Frontiers of Gastrointestinal Research. Vol. 26. Basel: Karger; 2010:59-71.
ERCP是MRCP不能完全替代的诊断或治疗的重要手段(如胆管细胞刷诊断胆管恶性病变,胆管取石,以及胆管狭窄的扩张术)。[25]Chapman R, Fevery J, Kalloo A, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51:660-678.http://onlinelibrary.wiley.com/doi/10.1002/hep.23294/fullhttp://www.ncbi.nlm.nih.gov/pubmed/20101749?tool=bestpractice.com[36]de Rougemont O, Dutkowski P, Clavien PA. Clinical update on inflammatory disorders of the GI tract: liver transplantation. In: Mayerle J, Tilg H, eds. Clinical update on inflammatory disorders of the gastrointestinal tract. Frontiers of Gastrointestinal Research. Vol. 26. Basel: Karger; 2010:59-71.
骨密度检测
所有患者一旦诊断,应每隔2-3年,完善骨密度检查以排除肝性骨营养不良。[37]Zein CO, Jorgensen RA, Clarke B, et al. Alendronate improves bone mineral density in primary biliary cirrhosis: a randomized placebo-controlled trial. Hepatology. 2005;42:762-771.http://onlinelibrary.wiley.com/doi/10.1002/hep.20866/fullhttp://www.ncbi.nlm.nih.gov/pubmed/16175618?tool=bestpractice.com[38]Collier J. Bone disorders in chronic liver disease. Hepatology. 2007;46:1271-1278.http://onlinelibrary.wiley.com/doi/10.1002/hep.21852/fullhttp://www.ncbi.nlm.nih.gov/pubmed/17886334?tool=bestpractice.com[25]Chapman R, Fevery J, Kalloo A, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51:660-678.http://onlinelibrary.wiley.com/doi/10.1002/hep.23294/fullhttp://www.ncbi.nlm.nih.gov/pubmed/20101749?tool=bestpractice.com
结肠镜检查
合并炎症性肠病(IBD)患者由于发生结直肠癌的风险很大,应定期进行结肠镜检查。[39]Vleggaar FP, Lutgens MW, Claessen MM, et al. Review article: the relevance of surveillance endoscopy in long-lasting inflammatory bowel disease. Aliment Pharmacol Ther. 2007;26(suppl 2):47-52.http://www.ncbi.nlm.nih.gov/pubmed/18081648?tool=bestpractice.com[25]Chapman R, Fevery J, Kalloo A, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51:660-678.http://onlinelibrary.wiley.com/doi/10.1002/hep.23294/fullhttp://www.ncbi.nlm.nih.gov/pubmed/20101749?tool=bestpractice.com
组织学
肝活检可帮助诊断PSC但并不是必需的,因症状、实验室检查和影像学检查已经可以诊断PSC。仅有1.3%已由胆管造影诊断PSC的患者能从肝活检受益。[40]Burak KW, Angulo P, Lindor KD. Is there a role for liver biopsy in primary sclerosing cholangitis? Am J Gastroenterol. 2003;98:1155-1158.http://www.ncbi.nlm.nih.gov/pubmed/12809842?tool=bestpractice.com然而,推荐肝活检用于小胆管PSC(胆管造影表现正常但实验室及组织学检查为PSC)或评估合并症。另外,肝活检可用于疾病分期(临床表现不明显的肝硬化)。[25]Chapman R, Fevery J, Kalloo A, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51:660-678.http://onlinelibrary.wiley.com/doi/10.1002/hep.23294/fullhttp://www.ncbi.nlm.nih.gov/pubmed/20101749?tool=bestpractice.com
PSC的病理学改变是纤维化-梗阻性胆管炎,但在进行肝活检的患者中仅有<12%的患者有此表现。[41]Wiesner RH, LaRusso NF, Ludwig J, et al. Comparison of the clinicopathologic features of primary sclerosing cholangitis and primary biliary cirrhosis. Gastroenterology. 1985;88:108-114.http://www.ncbi.nlm.nih.gov/pubmed/3880553?tool=bestpractice.com其他的病理学改变是非特异性的:汇管区纤维化、炎症、部分门脉区胆管缺失(简称局部胆管缺失)而其他门脉区胆管增生。[42]Ludwig J, Barham SS, LaRusso NF, et al. Morphologic features of chronic hepatitis associated with primary sclerosing cholangitis and chronic ulcerative colitis. Hepatology. 1981;1:632-640.http://www.ncbi.nlm.nih.gov/pubmed/7308996?tool=bestpractice.com
在行胆道的介入性检查时,脱落细胞学有助于排除胆管癌,尽管发现率仅为18%。[43]Baron TH, Harewood GC, Rumalla A, et al. A prospective comparison of digital image analysis and routine cytology for the identification of malignancy in biliary tract strictures. Clin Gastroenterol Hepatol. 2004;2:214-219.http://www.ncbi.nlm.nih.gov/pubmed/15017605?tool=bestpractice.com胆管癌诊断较困难,需要结合肿瘤标志物CA19-9、影像学等检查,和潜在的新检测技术,如组织学的荧光原位杂交。[25]Chapman R, Fevery J, Kalloo A, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51:660-678.http://onlinelibrary.wiley.com/doi/10.1002/hep.23294/fullhttp://www.ncbi.nlm.nih.gov/pubmed/20101749?tool=bestpractice.com
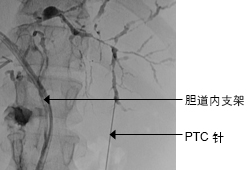 [Figure caption and citation for the preceding image starts]: 某患者的ERCP典型表现:肝内外胆管的多灶性狭窄Dr Kris Kowdley 收藏的资料 [Citation ends].
[Figure caption and citation for the preceding image starts]: 某患者的ERCP典型表现:肝内外胆管的多灶性狭窄Dr Kris Kowdley 收藏的资料 [Citation ends].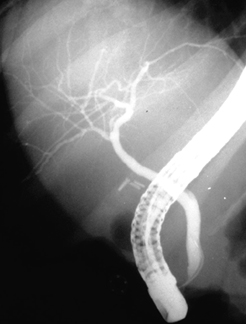 [Figure caption and citation for the preceding image starts]: 正常ECCPDr Michael Saunders 收藏的资料 [Citation ends].
[Figure caption and citation for the preceding image starts]: 正常ECCPDr Michael Saunders 收藏的资料 [Citation ends]. [Figure caption and citation for the preceding image starts]: 正常胆管造影-胰腺造影图Dr Michael Saunders 收藏的资料 [Citation ends].
[Figure caption and citation for the preceding image starts]: 正常胆管造影-胰腺造影图Dr Michael Saunders 收藏的资料 [Citation ends].