诊断中央气道阻塞(CAO)要结合病史(典型但非特异症状)和体格检查的特点,生理学,影像学和内镜检查的结果。最终,气管支气管阻塞的诊断需支气管镜下直视下观察诊断。
气道严重阻塞伴有急迫的窒息感,需要紧急行动迅速开放气道,解除阻塞。[17]Bolliger CT, Sutedja TG, Strausz J, et al. Therapeutic bronchoscopy with immediate effect: laser, electrocautery, argon plasma coagulation and stents. Eur Respir J. 2006;27:1258-1271.http://erj.ersjournals.com/content/27/6/1258.fullhttp://www.ncbi.nlm.nih.gov/pubmed/16772389?tool=bestpractice.com由于此类患者临床表现紧急,常规的初步检查(如高分辨率CT,肺功能)和诊断性可弯曲支气管镜检查可能难以进行。因此,在实践中,由于急性的危重情况非常常见,大多数检查,特别是肺功能检查,只能在少数患者实施。
临床病史
CAO可出现急性致命性情况,如突然发生的窒息感或渐进加重的呼吸症状。虽然不是所有患者都有病史,但在情况许可下收集详细临床病史对于诊断是必要的。
既往史和手术史
必须仔细回顾既往病史,并获得先前病历资料。[54]Brodsky JB. Bronchoscopic procedures for central airway obstruction. J Cardiothorac Vasc Anesth. 2003;17:638-646.http://www.ncbi.nlm.nih.gov/pubmed/14579222?tool=bestpractice.com
任何现在的或既往的恶性肿瘤病史都需要详细分析,大多数恶性CAO患者都是终末期原发性肿瘤患者或是既往化疗后肿瘤复发患者。[17]Bolliger CT, Sutedja TG, Strausz J, et al. Therapeutic bronchoscopy with immediate effect: laser, electrocautery, argon plasma coagulation and stents. Eur Respir J. 2006;27:1258-1271.http://erj.ersjournals.com/content/27/6/1258.fullhttp://www.ncbi.nlm.nih.gov/pubmed/16772389?tool=bestpractice.com此外患者恶性肿瘤的家族史也应关注。
需要机械通气的危重疾病史,有或没有外伤后气管插管或气管切开史务必要询问。
既往外科手术史,如肺切除术,肺移植术,或头颈部外科手术史必须询问。
患有风湿性疾病是重要的线索,如肉芽肿性多血管炎(韦格纳肉芽肿)和复发性多软骨炎。
某些感染性疾病,如结核或组织胞浆菌病增加了气道狭窄的风险,急性细菌性气管炎累及声门下区(如白喉)因黏膜水肿增厚,伴化脓性渗出液也可以引起气道阻塞。
共患疾病非常重要,CAO患者常患有多种疾病。吸烟,糖尿病或高血压和美国麻醉医师协会(ASA)量表较高评分均与治疗相关的并发症有关,如术中出血和低氧血症等。[55]Reddy C, Majid A, Michaud G, et al. Gas embolism following bronchoscopic argon plasma coagulation: a case series. Chest. 2008;134:1066-1069.http://www.ncbi.nlm.nih.gov/pubmed/18988782?tool=bestpractice.com
误吸风险的评估
症状
CAO患者一般症状严重且生活质量差。CAO症状多样且非特异,患者最常主诉的是呼吸急促和咳嗽,其他经常出现的是咯血,声嘶,胸部不适,端坐呼吸和吞咽困难。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com[2]Beamis JF Jr. Interventional pulmonology techniques for treating malignant large airway obstruction: an update. Curr Opin Pulm Med. 2005;11:292-295.http://www.ncbi.nlm.nih.gov/pubmed/15928494?tool=bestpractice.com[8]Mehta AC, Harris RJ, De Boer GE. Endoscopic management of benign airway stenosis. Clin Chest Med. 1995;16:401-413.http://www.ncbi.nlm.nih.gov/pubmed/8521696?tool=bestpractice.com[20]Seijo LM, Sterman DH. Interventional pulmonology. N Engl J Med. 2001;344:740-749.http://www.ncbi.nlm.nih.gov/pubmed/11236779?tool=bestpractice.com[21]Lee P, Kupeli E, Mehta AC. Therapeutic bronchoscopy in lung cancer: laser therapy, electrocautery, brachytherapy, stents, and photodynamic therapy. Clin Chest Med. 2002;23:241-256.http://www.ncbi.nlm.nih.gov/pubmed/11901914?tool=bestpractice.com[30]Dutau H, Toutblanc B, Lamb C, et al. Use of the Dumon Y-stent in the management of malignant disease involving the carina: a retrospective review of 86 patients. Chest. 2004;126:951-958.http://www.ncbi.nlm.nih.gov/pubmed/15364778?tool=bestpractice.com[54]Brodsky JB. Bronchoscopic procedures for central airway obstruction. J Cardiothorac Vasc Anesth. 2003;17:638-646.http://www.ncbi.nlm.nih.gov/pubmed/14579222?tool=bestpractice.com[56]Wahidi MM, Herth FJ, Ernst A. State of the art: interventional pulmonology. Chest. 2007;131:261-274.http://www.ncbi.nlm.nih.gov/pubmed/17218585?tool=bestpractice.com[57]Jabbardarjani H, Herth F, Kiani A, et al. Central airway obstruction masquerading as difficult-to-treat asthma: A retrospective study. J Bronchology Interv Pulmonol. 2009;16:6-9.http://www.ncbi.nlm.nih.gov/pubmed/23168459?tool=bestpractice.com
呼吸急促是较晚期的体征,在休息时或劳力时都会出现,有时也会因肺内巨大肿瘤压迫气道表现出体位相关的侧卧位用力呼吸包括(端坐呼吸),且吸入支气管舒张剂无效。气促程度与气道阻塞程度不一定相关。
咳嗽一般为慢性持续性干咳,但也可表现为吸入异物后的突发咳嗽,发生阻塞性肺炎时则多为伴有痰或脓痰的咳嗽。
如果气道轻度阻塞,气流无明显受限,患者可无症状。但当气道轻度狭窄伴急性呼吸系统感染时,气道黏膜水肿和气道分泌物聚集可明显减小狭窄部位管腔大小,导致呼吸症状迅速恶化。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com
当气流受限严重时,患者表现出症状,54%的气管狭窄患者会感到呼吸窘迫。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com劳力性呼吸困难出现时气管直径一定< 8mm,当直径<5mm时休息时就会出现呼吸困难。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com[54]Brodsky JB. Bronchoscopic procedures for central airway obstruction. J Cardiothorac Vasc Anesth. 2003;17:638-646.http://www.ncbi.nlm.nih.gov/pubmed/14579222?tool=bestpractice.com[56]Wahidi MM, Herth FJ, Ernst A. State of the art: interventional pulmonology. Chest. 2007;131:261-274.http://www.ncbi.nlm.nih.gov/pubmed/17218585?tool=bestpractice.com当合并其他肺部疾病(如慢阻肺),气道阻塞程度很轻时即可出现症状。
突发的呼吸困难提示可能是异物吸入。因成人多数误吸的异物并不会完全阻塞气道或仅仅嵌住了远端气道(右下叶支气管最常见),所以成人异物误吸后只有一小部分患者出现典型的三联征,如咳嗽,喘息和哽咽感。[45]Rafanan AL, Mehta AC. Adult airway foreign body removal: what's new? Clin Chest Med. 2001;22:319-330.http://www.ncbi.nlm.nih.gov/pubmed/11444115?tool=bestpractice.com但是,儿童异物吸入常阻塞中央气道,所以此三联征比成人更多见。[45]Rafanan AL, Mehta AC. Adult airway foreign body removal: what's new? Clin Chest Med. 2001;22:319-330.http://www.ncbi.nlm.nih.gov/pubmed/11444115?tool=bestpractice.com
咯血常见,尤其是病变在气道内时,可以是大量咯血,但多数报道是轻度到中度的咯血。引起咯血的病因包括肿瘤如鳞状细胞癌,原发于气道肿瘤(类癌和腺样囊性癌),肿瘤支气管内转移,感染(结核),炎症性疾病(如韦格纳肉芽肿)和良性气道肿瘤(如错构瘤)。慢性支气管炎患者常痰中带血丝,脓性分泌物,有时会被误诊为CAO。[58]Israel RH, Poe RH. Hemoptysis. Clin Chest Med. 1987;8:197-205.http://www.ncbi.nlm.nih.gov/pubmed/3621874?tool=bestpractice.com
气道恶性肿瘤压迫食道或食道肿瘤伴有支气管受侵时,患者可同时出现吞咽困难。
气管插管继发的气管狭窄,多于拔管后5周内出现呼吸急促,咳嗽和声嘶。声嘶也可能与上气道恶性肿瘤有关。
反复发生肺炎是常见的,表现为经常出现的呼吸困难,咳脓痰,发热和畏寒。[57]Jabbardarjani H, Herth F, Kiani A, et al. Central airway obstruction masquerading as difficult-to-treat asthma: A retrospective study. J Bronchology Interv Pulmonol. 2009;16:6-9.http://www.ncbi.nlm.nih.gov/pubmed/23168459?tool=bestpractice.com
在机械通气或气管切开患者,应关注肉芽组织增生相关的气管阻塞。以下情况的出现将提示这种气道阻塞的诊断,如撤机困难,呼吸机气道峰压高,逐渐出现喘鸣,人工气道拔除后或气切套管封堵后患者气促加重。
查体
呼吸系统检查
与CAO的位置,累及范围和病因有关,胸部听诊可闻及喘鸣,哮鸣音,局灶性湿啰音或实变体征。
当气道直径<5mm 时会出现喘鸣音,提示严重声门下或气管狭窄。[59]Hollingsworth HM. Wheezing and stridor. Clin Chest Med. 1987;8:231-240.http://www.ncbi.nlm.nih.gov/pubmed/3304813?tool=bestpractice.com吸气相喘鸣音提示在声带水平或声带以上位置的胸腔外气管阻塞,闻及最明显的部位在颈部。[14]Aboussouan LS, Stoller JK. Diagnosis and management of upper airway obstruction. Clin Chest Med. 1994;15:35-53.http://www.ncbi.nlm.nih.gov/pubmed/8200192?tool=bestpractice.com呼气相喘鸣音可能是因为胸腔内气道阻塞导致。[54]Brodsky JB. Bronchoscopic procedures for central airway obstruction. J Cardiothorac Vasc Anesth. 2003;17:638-646.http://www.ncbi.nlm.nih.gov/pubmed/14579222?tool=bestpractice.com吸气呼气双相喘鸣音出现在声门下或气管狭窄。[14]Aboussouan LS, Stoller JK. Diagnosis and management of upper airway obstruction. Clin Chest Med. 1994;15:35-53.http://www.ncbi.nlm.nih.gov/pubmed/8200192?tool=bestpractice.com增加气流的动作如过度通气,可以加重喘鸣音,颈部弯曲动作可以改变喘鸣音的强度。[31]Fishman AP, Elias JA, Fishman JA, et al. Fishman's pulmonary diseases and disorders. 4th ed. New York, NY: McGraw-Hill; 2008.
哮鸣音可出现在吸气相或呼气相,哮鸣音定位并不一定能反映气道阻塞的位置,其可在气管上段或肺野中出现。[59]Hollingsworth HM. Wheezing and stridor. Clin Chest Med. 1987;8:231-240.http://www.ncbi.nlm.nih.gov/pubmed/3304813?tool=bestpractice.com单侧哮鸣音提示阻塞位于隆突以下远端气道。哮鸣音亦可与体位相关,一般对支气管舒张剂治疗无反应。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com[8]Mehta AC, Harris RJ, De Boer GE. Endoscopic management of benign airway stenosis. Clin Chest Med. 1995;16:401-413.http://www.ncbi.nlm.nih.gov/pubmed/8521696?tool=bestpractice.com
严重CAO时,患者可出现显著焦虑,呼吸急促,心动过速,辅助呼吸肌用力,胸骨内陷,呼吸时颈部伸展,紫绀,甚至呼吸骤停。
初步影像学
每个疑诊CAO的患者均应接受胸片检查。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com[60]Simoff MJ, Sterman DH, Ernst A (eds). Thoracic endoscopy. Advances in interventional pulmonology. Malden, MA: Blackwell; 2006.胸片可以发现明显的病变,如因邻近病变引起气管偏曲,虽然不常做诊断,但发现气管和主支气管异常的敏感率约66%。[13]Santacruz JF, Mehta AC. Airway complications and management after lung transplantation: ischemia, dehiscence, and stenosis. Proc Am Thorac Soc. 2009;6:79-93.http://www.ncbi.nlm.nih.gov/pubmed/19131533?tool=bestpractice.com[61]Collins J, Stern EJ. Chest radiology. The essentials. 2nd ed. Philadelphia, PA: Wolters Kluwer; 2008.
胸片气道阻塞的标志是呼气相胸片上出现气体陷闭。气体陷闭的特点是呼气时肺内容积不减少,与吸气相比较,呼气时透亮度增加,纵隔向无气体陷闭侧移位。出现气体陷闭的原因是支气管内阻塞病变引起单向阀样阻塞。[61]Collins J, Stern EJ. Chest radiology. The essentials. 2nd ed. Philadelphia, PA: Wolters Kluwer; 2008.
气管支气管内充盈缺损,提示黏液堵塞或肿物。其他常见影像学异常,尤其是中央型鳞状细胞癌,可表现为阻塞性肺炎和肺不张。成人出现肺叶不张,应考虑中央型肿物阻塞。[61]Collins J, Stern EJ. Chest radiology. The essentials. 2nd ed. Philadelphia, PA: Wolters Kluwer; 2008.另外,肺叶或全肺萎陷应考虑肿瘤相关的主支气管阻塞。
'金色S征'与中央气道肿物阻塞有关。肿物周围肺叶萎陷,因为中央气道肿物导致中央部分肺叶不能萎陷。邻近叶间裂向周围凹陷而向中心突出,叶裂形状呈现'S'或‘反S'形。[61]Collins J, Stern EJ. Chest radiology. The essentials. 2nd ed. Philadelphia, PA: Wolters Kluwer; 2008. [Figure caption and citation for the preceding image starts]: 胸部CT(左图)金色S征或反S征,黄线标记。可弯曲支气管镜(右图)显示中央气道阻塞病变位于左主支气管。由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 胸部CT(左图)金色S征或反S征,黄线标记。可弯曲支气管镜(右图)显示中央气道阻塞病变位于左主支气管。由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
支气管镜检查
可弯曲支气管镜或硬质支气管镜是诊断CAO,评估气道阻塞的最特异和敏感的检查。[8]Mehta AC, Harris RJ, De Boer GE. Endoscopic management of benign airway stenosis. Clin Chest Med. 1995;16:401-413.http://www.ncbi.nlm.nih.gov/pubmed/8521696?tool=bestpractice.com[20]Seijo LM, Sterman DH. Interventional pulmonology. N Engl J Med. 2001;344:740-749.http://www.ncbi.nlm.nih.gov/pubmed/11236779?tool=bestpractice.com[60]Simoff MJ, Sterman DH, Ernst A (eds). Thoracic endoscopy. Advances in interventional pulmonology. Malden, MA: Blackwell; 2006.[62]Jeon K, Kim H, Yu CM, et al. Rigid bronchoscopic intervention in patients with respiratory failure caused by malignant central airway obstruction. J Thorac Oncol. 2006;1:319-323.http://www.ncbi.nlm.nih.gov/pubmed/17409877?tool=bestpractice.com
支气管镜检查可以明确病变的定位,形态,腔内病变数量,是否存在腔外压迫,以及病变的直径和深度,也可以评估周围情况尤其是阻塞远端气道。此外,需要时可以进行组织病理诊断。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com
诊断性的可弯曲支气管镜检查具有一定的风险和弊端,开展时需要注意。其并不能完全评估气道外病变或阻塞远端气道的情况,在严重气道阻塞时进行支气管镜检查难以操作且有潜在的风险,因为支气管镜本身可能加重已阻塞管腔的狭窄,减少通气。[17]Bolliger CT, Sutedja TG, Strausz J, et al. Therapeutic bronchoscopy with immediate effect: laser, electrocautery, argon plasma coagulation and stents. Eur Respir J. 2006;27:1258-1271.http://erj.ersjournals.com/content/27/6/1258.fullhttp://www.ncbi.nlm.nih.gov/pubmed/16772389?tool=bestpractice.com可弯曲支气管镜操作后,如果在气道狭窄部位出现分泌物,水肿或出血,会导致狭窄的管腔有进一步阻塞的风险。操作时给予中度镇静可以减少通气,降低呼吸肌紧张性,但增加了气道潜在的不安全因素。基于上述原因,为CAO患者进行诊断性支气管镜检查时,医疗团队需要配备先进的气道介入治疗设备。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com
CAO的支气管镜介入治疗通常包括2个步骤,首先是诊断性探查,然后进行治疗性支气管镜操作。可弯曲支气管镜操作技术可以作为病情相对稳定患者的主要治疗,它也是大多数支气管镜下介入治疗操作使用的技术。
对于呼吸近乎停止的严重气道阻塞病例,可弯曲支气管镜等检查性的操作不大可能进行,应该直接进行硬质支气管镜操作。[60]Simoff MJ, Sterman DH, Ernst A (eds). Thoracic endoscopy. Advances in interventional pulmonology. Malden, MA: Blackwell; 2006.硬质支气管镜操作是一项安全有效的气道保护技术,对于评估和治疗CAO非常有帮助,在诊断和治疗性气道介入操作时可以保证气道通气和氧合。[15]Bolliger CT, Mathur PN, Beamis JF, et al. ERS/ATS statement on interventional pulmonology. European Respiratory Society. Eur Respir J. 2002;19:356-373.http://erj.ersjournals.com/content/19/2/356.fullhttp://www.ncbi.nlm.nih.gov/pubmed/11866017?tool=bestpractice.com[60]Simoff MJ, Sterman DH, Ernst A (eds). Thoracic endoscopy. Advances in interventional pulmonology. Malden, MA: Blackwell; 2006.[62]Jeon K, Kim H, Yu CM, et al. Rigid bronchoscopic intervention in patients with respiratory failure caused by malignant central airway obstruction. J Thorac Oncol. 2006;1:319-323.http://www.ncbi.nlm.nih.gov/pubmed/17409877?tool=bestpractice.com[63]Ayers ML, Beamis JF Jr. Rigid bronchoscopy in the twenty-first century. Clin Chest Med. 2001;22:355-364.http://www.ncbi.nlm.nih.gov/pubmed/11444118?tool=bestpractice.com[64]Ko-Pen W, Mehta AC, Turner JF. Flexible bronchoscopy. 2nd ed. Malden, MA: Blackwell; 2004.[65]Ernst A, Silvestri GA, Johnstone D. Interventional pulmonary procedures: guidelines from the American College of Chest Physicians. Chest. 2003;123:1693-1717.http://www.ncbi.nlm.nih.gov/pubmed/12740291?tool=bestpractice.com此外,必要时可弯曲支气管镜可以通过硬镜进入气道。
高级影像学
计算机体断层扫描(包括高分辨率CT,多排CT和虚拟支气管镜)
胸部CT是评估气道情况的最准确的无创性检查方法,可用于CAO的诊断和制定治疗计划。
建议采用高分辨率CT诊断CAO。[60]Simoff MJ, Sterman DH, Ernst A (eds). Thoracic endoscopy. Advances in interventional pulmonology. Malden, MA: Blackwell; 2006.对于诊断气管和主支气管异常病变,CT优于胸片,其敏感度达97%。[61]Collins J, Stern EJ. Chest radiology. The essentials. 2nd ed. Philadelphia, PA: Wolters Kluwer; 2008.
CT能探及气道阻塞病变的类型(腔内型,腔外型或混合型),阻塞远端是否通畅,病变的长度和直径,与周围组织如血管的关系。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com
气管狭窄分为管腔局灶型或弥漫型狭窄。虽然CT可以准确地显示出气管壁和管腔的解剖结构,但对气道狭窄的细微变化识别能力有限,常低估气管和支气管狭窄的长度。
CT可以明确地显示气管腔内肿瘤、气管受压以及其他良性弥漫性气管病变征象。[66]Chung JH, Kanne JP. Multidetector-row computed tomography of diffuse tracheal disease: pictorial review. J Bronchol Interv Pulmonol. 2009;16:28-36.http://www.ncbi.nlm.nih.gov/pubmed/23168465?tool=bestpractice.com阻塞性肺炎,肺不张以及肺叶萎陷也可在CT上明确地观察到。
气管支气管内充盈缺损,提示气道内占位性病变(如肿瘤或黏液),CT可以明确地定位中央气道内或附近的病变部位和受累范围。
多层CT(MDCT)可以在一次呼吸屏气期间收集到层厚0.5-2mm CT的所有相邻和/或相交的层面信息,增强了探及气道病变的能力,如支气管内肿瘤(包括中央气道肿瘤),而传统CT使用7-10mm层厚可能会漏诊。[37]Naidich DP, Webb WR, Muller NL, et al. Computed tomography and magnetic resonance of the thorax. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007. [Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:肺窗证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:肺窗证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends]. [Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:纵隔窗证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:纵隔窗证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
MDCT还可提供高质量的多平面重建技术(MPRs),表面三维显示以及内部透视体现容积(称为虚拟支气管镜),从而能更准确地估算出气管支气管病变的长度。[37]Naidich DP, Webb WR, Muller NL, et al. Computed tomography and magnetic resonance of the thorax. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007.[67]Boiselle PM. Imaging of the large airways. Clin Chest Med. 2008;29:181-193.http://www.ncbi.nlm.nih.gov/pubmed/18267191?tool=bestpractice.com [Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:冠状位重建证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:冠状位重建证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends]. [Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:3维体绘制重建证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:3维体绘制重建证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends]. [Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:2维多平面重建(最小强度投影)证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:2维多平面重建(最小强度投影)证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
与可弯曲支气管镜可直接观察相比,虚拟支气管镜是无创性技术,它可以观察中央气道并探查阻塞支气管的病变(包括腔内和腔外)和局灶性支气管狭窄。[37]Naidich DP, Webb WR, Muller NL, et al. Computed tomography and magnetic resonance of the thorax. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007.[68]Finkelstein SE, Summers RM, Nguyen DM, et al. Virtual bronchoscopy for evaluation of malignant tumors of the thorax. J Thorac Cardiovasc Surg. 2002;123:967-972.http://www.ncbi.nlm.nih.gov/pubmed/12019383?tool=bestpractice.com[69]De Wever W, Bogaert J, Verschakelen JA. Virtual bronchoscopy: accuracy and usefulness - an overview. Semin Ultrasound CT MR. 2005;26:364-373.http://www.ncbi.nlm.nih.gov/pubmed/16274005?tool=bestpractice.com也有助于制定介入治疗计划,如气道置入支架。[69]De Wever W, Bogaert J, Verschakelen JA. Virtual bronchoscopy: accuracy and usefulness - an overview. Semin Ultrasound CT MR. 2005;26:364-373.http://www.ncbi.nlm.nih.gov/pubmed/16274005?tool=bestpractice.com
CT和MPRs可准确的探查到气管支气管狭窄的位置和程度,敏感性达93%%,特异性100%,准确性为94%。[70]Whyte RI, Quint LE, Kazerooni EA, et al. Helical computed tomography for the evaluation of tracheal stenosis. Ann Thorac Surg. 1995;60:27-30.http://www.ncbi.nlm.nih.gov/pubmed/7598617?tool=bestpractice.com对于发现肺移植术后支气管狭窄的准确性为94%。[71]Quint LE, Whyte RI, Kazerooni EA, et al. Stenosis of the central airways: evaluation by using helical CT with multiplanar reconstructions. Radiology. 1995;194:871-877.http://www.ncbi.nlm.nih.gov/pubmed/7862994?tool=bestpractice.com
胸部多层螺旋CT的吸气与呼气动态对比检查在诊断气管支气管软化方面非常有用。[12]Murgu SD, Colt HG. Complications of silicone stent insertion in patients with expiratory central airway collapse. Ann Thorac Surg. 2007;84:1870-1877.http://www.ncbi.nlm.nih.gov/pubmed/18036901?tool=bestpractice.com与吸气时比较,呼气时中央气道的横断面面积减少>50%,定义为气道软化。[67]Boiselle PM. Imaging of the large airways. Clin Chest Med. 2008;29:181-193.http://www.ncbi.nlm.nih.gov/pubmed/18267191?tool=bestpractice.com [Figure caption and citation for the preceding image starts]: 动力性气道塌陷:A.吸气时支气管镜下所见;B.呼气时支气管镜下可见动力性气道塌陷;C.吸气时胸部CT显示正常气道;D. 呼气时胸部CT显示气道明显塌陷由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 动力性气道塌陷:A.吸气时支气管镜下所见;B.呼气时支气管镜下可见动力性气道塌陷;C.吸气时胸部CT显示正常气道;D. 呼气时胸部CT显示气道明显塌陷由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
胸部MRI
胸部MRI用于评估喉部,气管近端,纵隔和肺门肿物,易于分辨血管和软组织肿物。[60]Simoff MJ, Sterman DH, Ernst A (eds). Thoracic endoscopy. Advances in interventional pulmonology. Malden, MA: Blackwell; 2006.
其可以无需借助造影剂,探及多层面胸部图像,特别是善于探查气道周围的血管结构,例如可能压迫气管的血管环或动脉瘤。[31]Fishman AP, Elias JA, Fishman JA, et al. Fishman's pulmonary diseases and disorders. 4th ed. New York, NY: McGraw-Hill; 2008.
肺功能检查
肺量测定和流量-容量环分析是评估CAO的重要部分,条件许可时都应该进行。
流量-容量环(FVL)
评估FVL的形状可以识别上气道阻塞(UAO)并加以分类,可分为动力性胸腔外(非固定或可变性),动力性胸腔内(非固定或可变性)和固定性上气道阻塞。气管分为胸腔外段(胸骨上切记以上的三分之一气管)和胸腔内段(胸骨上切记以下的三分之二气管)两部分。
动力性胸腔外上气道阻塞时,用力吸气时胸腔外气管受压加重,气流变慢,流量-容量环吸气支呈平台状。[13]Santacruz JF, Mehta AC. Airway complications and management after lung transplantation: ischemia, dehiscence, and stenosis. Proc Am Thorac Soc. 2009;6:79-93.http://www.ncbi.nlm.nih.gov/pubmed/19131533?tool=bestpractice.com动力性胸腔内气道阻塞时,用力呼气时胸腔内气管可受压加重,气流变慢,故产生FVL平台型呼气支。[13]Santacruz JF, Mehta AC. Airway complications and management after lung transplantation: ischemia, dehiscence, and stenosis. Proc Am Thorac Soc. 2009;6:79-93.http://www.ncbi.nlm.nih.gov/pubmed/19131533?tool=bestpractice.com固定性上气道阻塞病变,吸气相和呼气相跨壁压的变化不改变气流受限情况,因此在吸气和呼气环部分均产生平台。[13]Santacruz JF, Mehta AC. Airway complications and management after lung transplantation: ischemia, dehiscence, and stenosis. Proc Am Thorac Soc. 2009;6:79-93.http://www.ncbi.nlm.nih.gov/pubmed/19131533?tool=bestpractice.com [Figure caption and citation for the preceding image starts]: 动力性(非固定性或可变性)胸腔外上气道阻塞:流量-容量环显示用力吸气时吸气相呈‘平台’样改变由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 动力性(非固定性或可变性)胸腔外上气道阻塞:流量-容量环显示用力吸气时吸气相呈‘平台’样改变由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends]. [Figure caption and citation for the preceding image starts]: 动力性(非固定性或可变性)胸腔内上气道阻塞:流量-容量环显示用力呼气时呼气相呈‘平台’样改变由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 动力性(非固定性或可变性)胸腔内上气道阻塞:流量-容量环显示用力呼气时呼气相呈‘平台’样改变由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].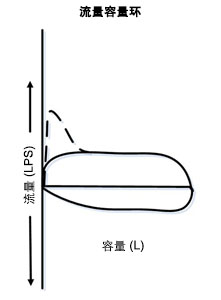 [Figure caption and citation for the preceding image starts]: 固定性上气道阻塞:流量-容量环显示吸气和呼气相均呈‘平台’样改变由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 固定性上气道阻塞:流量-容量环显示吸气和呼气相均呈‘平台’样改变由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
FVL需考虑气道的动力性变化特点,例如肺容量测定时因用力吸气和呼气动作气道跨壁压的变化,导致上气道管径改变。
只有当气管阻塞的管径严重狭窄时(直径8-10mm),FVL才会出现典型的曲线,故FVL对于诊断UAO非常不敏感。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com[14]Aboussouan LS, Stoller JK. Diagnosis and management of upper airway obstruction. Clin Chest Med. 1994;15:35-53.http://www.ncbi.nlm.nih.gov/pubmed/8200192?tool=bestpractice.com[31]Fishman AP, Elias JA, Fishman JA, et al. Fishman's pulmonary diseases and disorders. 4th ed. New York, NY: McGraw-Hill; 2008.
对于已经患有肺病的患者(如慢阻肺),因为存在多部位气流阻塞,不能吹出高流量气流,FVL可能不出现气道狭窄的图形。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com因此在此类患者,FVL识别中央气道狭窄病变的能力更差。[14]Aboussouan LS, Stoller JK. Diagnosis and management of upper airway obstruction. Clin Chest Med. 1994;15:35-53.http://www.ncbi.nlm.nih.gov/pubmed/8200192?tool=bestpractice.com
呼吸量测定
由于呼吸量测定可能诱发呼吸衰竭,对于CAO患者合并呼吸窘迫或加重时不要进行呼吸量测定。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com
当气道阻塞部位直径减小到6mm时,一秒钟用力呼气量(FEV1)才会出现显著下降,因此FVL曲线变化可能早于FEV1出现异常。[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com
与FEV1相比,最大呼气流速(PEFR)和最大自主通气量(MVV)诊断UAO的敏感性更高。
在用力肺容量测定时,如果PEFR下降不成比例的显著低于FEV1下降时,应该怀疑UAO。[14]Aboussouan LS, Stoller JK. Diagnosis and management of upper airway obstruction. Clin Chest Med. 1994;15:35-53.http://www.ncbi.nlm.nih.gov/pubmed/8200192?tool=bestpractice.com[31]Fishman AP, Elias JA, Fishman JA, et al. Fishman's pulmonary diseases and disorders. 4th ed. New York, NY: McGraw-Hill; 2008.MVV与FEV1的比值小于25%常见于UAO,当MVV下降伴FEV1正常时,也应该考虑诊断UAO。[31]Fishman AP, Elias JA, Fishman JA, et al. Fishman's pulmonary diseases and disorders. 4th ed. New York, NY: McGraw-Hill; 2008.
支气管内超声(EBUS)
EBUS已经成功用于CAO的评估和其治疗计划的制定[1]Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med. 2004;169:1278-1297.http://www.ncbi.nlm.nih.gov/pubmed/15187010?tool=bestpractice.com,其可用于识别是否存在气道软骨外病变和气道受累的程度,并探查阻塞病变远端气道的情况。
 [Figure caption and citation for the preceding image starts]: 胸部CT(左图)金色S征或反S征,黄线标记。可弯曲支气管镜(右图)显示中央气道阻塞病变位于左主支气管。由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 胸部CT(左图)金色S征或反S征,黄线标记。可弯曲支气管镜(右图)显示中央气道阻塞病变位于左主支气管。由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends]. [Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:肺窗证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:肺窗证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends]. [Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:纵隔窗证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:纵隔窗证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends]. [Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:冠状位重建证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:冠状位重建证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends]. [Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:3维体绘制重建证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:3维体绘制重建证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends]. [Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:2维多平面重建(最小强度投影)证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 恶性支气管内阻塞的胸部多排CT:2维多平面重建(最小强度投影)证实右主支气管恶性肿瘤阻塞由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends]. [Figure caption and citation for the preceding image starts]: 动力性气道塌陷:A.吸气时支气管镜下所见;B.呼气时支气管镜下可见动力性气道塌陷;C.吸气时胸部CT显示正常气道;D. 呼气时胸部CT显示气道明显塌陷由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 动力性气道塌陷:A.吸气时支气管镜下所见;B.呼气时支气管镜下可见动力性气道塌陷;C.吸气时胸部CT显示正常气道;D. 呼气时胸部CT显示气道明显塌陷由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends]. [Figure caption and citation for the preceding image starts]: 动力性(非固定性或可变性)胸腔外上气道阻塞:流量-容量环显示用力吸气时吸气相呈‘平台’样改变由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 动力性(非固定性或可变性)胸腔外上气道阻塞:流量-容量环显示用力吸气时吸气相呈‘平台’样改变由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends]. [Figure caption and citation for the preceding image starts]: 动力性(非固定性或可变性)胸腔内上气道阻塞:流量-容量环显示用力呼气时呼气相呈‘平台’样改变由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 动力性(非固定性或可变性)胸腔内上气道阻塞:流量-容量环显示用力呼气时呼气相呈‘平台’样改变由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].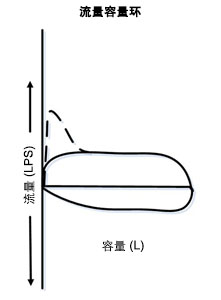 [Figure caption and citation for the preceding image starts]: 固定性上气道阻塞:流量-容量环显示吸气和呼气相均呈‘平台’样改变由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].
[Figure caption and citation for the preceding image starts]: 固定性上气道阻塞:流量-容量环显示吸气和呼气相均呈‘平台’样改变由 Jose Fernando Santacruz MD, FCCP, DAABIP 和 Erik Folch MD, MSc 提供;经许可后使用 [Citation ends].